Jacob Healthcare Center
4075 54Th St
San Diego, CA 92105 (619) 582-5168
Provider Type:
Nursing Facility
License Number:
90000093
At-A-Glance?
| Current | |
|---|---|
CMS 5-Star rating |  |
Special Focus Facility | No |
At-A-Glance
This section provides a quick overview of the description of the nursing home as well as the quality of the care provided. This includes some data that describes the nursing home capabilities as well as select long-stay and short-stay quality measures. All measures included in this section are also repeated in their respective sections – Facility Description, Staffing, Quality of Care, and Health and Safety Inspections.
Ratings on the Cal Long Term Care Compare (CLTCC) website are derived both from the federal Centers for Medicare & Medicaid Services (CMS) five-star quality rating system and select performance score ratings analyzed by the CLTCC team. For additional information on a nursing home, see the California Department of Public Health’s Licensing and Certification Program (L&C).
- CMS uses a five-star rating system where more stars indicate better quality.
- For any measures that are scored by the CLTCC team, click on the score badge for an explanation of the ratings.
CMS 5-Star rating (Data Source: CMS Provider Data: through 9/30/2025)
The U.S. Centers for Medicare & Medicaid Services (CMS) created a five-star quality rating system to help consumers, their families, and caregivers compare nursing homes more easily and to help identify areas about which you may want to ask questions. Nursing homes with five stars are considered to have well above average quality, and nursing homes with one star are considered to have well below average quality. For more information, see the CMS website.
Special Focus Facility (Data Source: CMS Provider Data: through 9/30/2025)
The U.S. Centers for Medicare & Medicaid Services (CMS) created the Special Focus Facility (SFF) initiative to stimulate systematic improvements in quality of care. CMS has found that a small number of nursing homes have more serious problems than most other nursing homes that have persisted over at least three years. CMS requires that SFF nursing homes be visited in person by survey teams twice as frequently as other nursing homes to ensure improvements are being made. CMS limits California to 6 nursing homes on the SFF list at one time. For more information, see the CMS website.
Facility Description?
| Current | State Average | |
|---|---|---|
Facility type | Freestanding |
NA |
Payments accepted | Medicare and Medicaid |
NA |
Number of beds | 128 |
97.0 |
Facility Description
Facility type (Data Source: CMS Provider Data; CDPH Licensed and Certified Healthcare Facility Listing: through 9/30/2025)
There are two basic types of skilled nursing facilities: freestanding or a distinct part of a hospital.
- Freestanding: Freestanding facilities provide 24-hour skilled nursing care to assist with short term recovery from a surgery, injury, or acute illness or provide on-going nursing home care for those who need more permanent long-term care.
- Distinct Part of acute care hospital: A Distinct Part facility is always associated with a hospital. It must be physically distinguishable from the hospital (separate address) and fiscally separate for cost reporting purposes. A Distinct Part facility provides the same services as a freestanding facility as well as treatment for acute illness or injury and intensive rehabilitation services. Most residents stay a brief time, usually a maximum of three weeks, and then are discharged to either a freestanding nursing home or back to their own home.
Payments accepted (Data Source: CDPH Licensed and Certified Healthcare Facility Listing: through 9/30/2025)
All nursing homes in California accept insurance payments directly from insurance companies (including private insurance and long-term care insurance). In addition, many are certified to receive payment from the Medicare program for short term stays defined as the first 100 days (about 3 and a half months) of care. Medicare pays most costs (excluding co-pays) for those who are Medicare beneficiaries. Medicare does not pay for stays beyond 100 consecutive days, at which point residents are considered to be long-term care residents. Some, but not all, facilities accept payment from the Medicaid program (Medi-Cal) for long-term residents with low incomes and few assets. If the resident does not qualify for Medi-Cal, they will be billed for the cost of care.
Number of beds (Data Source: CDPH Licensed and Certified Healthcare Facility Listing: through 9/30/2025)
This indicates the number of licensed beds distributed among private and shared rooms that have been certified to be paid for by Medicare and/or Medi-Cal.
Staffing?
| Current | State Average | |
|---|---|---|
CLTCC Staffing Rating |  (higher is better) (higher is better) |
NA |
Nursing staff turnover | 40% (lower is better) |
39.0% (lower is better) |
Percent of nursing staff who worked in the facility continuously for 12 months | 89% (higher is better) |
70.0% (higher is better) |
Staffing
CLTCC Staffing Rating (Data Source: Cal Long Term Care Compare: 1/1/2025 through 3/31/2025)
Most nursing homes in California care for a combination of people who are either recovering from a hospital stay or need long-term care. Evidence shows that staffing levels in nursing homes can affect the quality of care that residents receive in the nursing home. The CLTCC Staffing Rating shows whether the nursing home meets California’s minimum nurse staff hour requirements and whether it also provides enough hours of nursing care to meet the needs of its residents based on their severity of illness.
California Minimum Requirements: California law requires its nursing homes to provide at least 3.5 hours of direct nursing care per resident day, with at least 2.4 hours of that time coming from certified nursing assistants (CNAs). This does not mean that each resident gets 3.5 hours of nursing care every day because residents who are sicker or require complex care will need more hours of care per day while healthier residents will need less nursing care.
Expected Nursing Hours: The best nursing homes not only meet the state’s minimum requirement, but they also increase their staff hours based on the health conditions or severity of illness of their residents. The CLTCC rating includes the number of staff needed based on the severity of all residents in the nursing home during the measurement period. This calculation can help nursing homes estimate the expected nursing hours needed to care for all their residents’ needs. The number of hours may exceed California’s minimum staffing requirement.
Nursing homes that meet minimum nursing hour requirements and meet or go beyond expected nursing hours get higher ratings.
Rating definitions:
- Poor: Did not provide California’s minimum nurse staff hours requirement. Specifically – failed to meet the California minimum requirement for both CNAs and total nurse staffing.
- Below Average: Met only part of the state requirement. Specifically – met only ONE of the two state minimum staffing requirements, either CNA or total nurse staffing.
- Average: Met or exceeded the California minimum staffing hours, but did not meet the expected hours for either CNA hours or total nursing hours based on residents’ severity of illness.
- Above Average: Had enough staff to meet California’s minimum nurse staff hours requirement and met or exceeded expectations for either CNA hours or total staffing hours based on residents’ severity of illness.
- Superior: Met the state minimum requirements and met or exceeded expected hours for both CNA and total nurse staff hours based on residents’ severity of illness.
Nursing staff turnover (Data Source: CMS Provider Data: 1/1/2024 through 12/31/2024)
The turnover measure shows the percent of all nursing staff (registered nurses, licensed practical/vocational nurses, and certified nursing assistants) who stopped working at the nursing home over a 12-month period. When nursing staff is constantly changing, it may be stressful and disruptive for residents to receive care from new staff who are unfamiliar with their routines or special needs. Evidence shows that the lower the nursing staff turnover rate at a nursing facility, the better the quality, continuity, and stability of care. If a nursing home has high turnover, families should ask about the reasons and how it affects care.
Percent of nursing staff who worked in the facility continuously for 12 months (Data Source: LTC Facility Integrated Disclosure and Medi-Cal Cost Report Data: 1/1/2023 through 12/31/2023)
This measure reflects the percentage of all nursing staff (registered nurses, licensed practical/vocational nurses, and certified nursing assistants) who stayed in their job for the past 12 months. Nursing staff who remain in the nursing home are generally more satisfied with their jobs. Higher retention rates can be associated with higher quality of care because there is more stability of the nursing home workforce. If a nursing home has low staff retention, families should ask about the reasons and how it affects care.
Quality of Care?
| Current | State Average | |
|---|---|---|
Short-Stay Residents |
||
Rate of successful return to home and community from a nursing home | 56% (higher is better) |
51.0% (higher is better) |
Percentage of residents who are at or above an expected ability to move around at discharge | 57% (higher is better) |
48.0% (higher is better) |
Long-Stay Residents |
||
Percentage of long-stay residents who received an antipsychotic medication | 2% (lower is better) |
10.0% (lower is better) |
Percentage of long-stay residents with pressure ulcers | 6% (lower is better) |
5.0% (lower is better) |
Percentage of long-stay residents who lose too much weight | 3% (lower is better) |
4.3% (lower is better) |
Percentage of long-stay residents with new or worsened bowel or bladder incontinence | 2% (lower is better) |
12.0% (lower is better) |
Quality of Care
Short-Stay Residents
Percentage of successful return to home and community from a nursing home (Data source: CMS SNF Quality Reporting Program-Provider Data, 10/01/2021 – 09/30/2023)
This measure reports the percentage of short-stay residents admitted to the nursing home from a hospital who were then discharged to the community within 100 calendar days of admission, and who remained in the community for at least 30 consecutive days following discharge to the community. This measure is adjusted to be more fair among nursing homes because it takes into account characteristics about each resident like their age and how sick they are. If nursing homes have high numbers of residents who are readmitted to the hospital after discharge, it may indicate they are not adequately preparing residents for discharge or appropriately evaluating residents’ readiness to successfully care for themselves at home.
Percentage of residents who are at or above an expected ability to care for themselves and move around at discharge. (Data source: CMS SNF Quality Reporting Program-Provider Data, 04/01/2023 – 03/31/2024)
This measure reports the percentage of residents who are at or above their expected ability to care for themselves and move around when discharged from the SNF. Reducing difficulties with activities like eating, toileting, and moving around can improve residents’ quality of life. This measure is adjusted to be more fair among nursing homes because it takes into account characteristics about each resident like their age and how sick they are.
Long-Stay Residents
Percentage of long-stay residents who received an antipsychotic medication (Data Source: CMS MDS Quality Measures, 10/01/2023 – 09/30/2024)
Antipsychotic medications are used to treat a very specific group of mental health conditions such as schizophrenia; however, these drugs historically have been used to manage agitated behaviors in residents without schizophrenia or other appropriate medical conditions. This measure reports the percentage of long-stay residents who received an antipsychotic medication during the reporting period. This class of medications can cause serious harm and should not be given to control mood or behavior, particularly in residents with dementia. Those who have a diagnosis of schizophrenia, Tourette’s syndrome, or Huntington’s disease were excluded from this measure as antipsychotics are appropriate for these residents. Nursing homes should employ alternative methods to reduce agitation such as increased exercise, improved pain management, music therapy, and other non-drug interventions. High rates of antipsychotic use may indicate poor quality of care. Nursing homes should have non-pharmacological programs to manage resident behavioral issues. This measure is not adjusted for resident characteristics.
Percentage of long-stay residents with pressure ulcers (Data Source: CMS MDS Quality Measures, 04/01/2023 – 03/31/2024)
Pressure ulcers (also known as pressure injuries or sores) are areas of damaged skin caused by the resident staying in one position for too long; prolonged pressure in that area causes breakdown in the skin and underlying tissue resulting in a pressure sore, ulcer or open wound. Long-stay residents who have at least one of the following conditions are considered to be at high-risk for pressure ulcers: impaired mobility (difficulty moving), difficulty staying nourished (poor nutrition), or in a coma. This measure reports high-risk, long-stay residents who have pressure ulcers/injuries. These residents are dependent upon the nursing staff to turn and reposition them frequently to avoid pressure ulcers/injuries. Nursing homes should have a strong pressure ulcer/injury program that emphasizes frequent repositioning in residents at high risk. This measure is not adjusted for resident characteristics.
Percentage of long-stay residents who lose too much weight (Data Source: CMS MDS Quality Measures, 10/01/2023 – 9/30/2024)
Unexpected or unintentional weight loss is often associated with poor health outcomes and could be associated with an underlying illness. However, it may also be associated with certain medications, difficulty chewing or swallowing food, poor dental health, and depression among other causes. Nursing home staff should monitor each resident’s weight regularly and if there is unintentional, significant weight loss (5% or more in the last month or 10% or more in the last 6 months), they should notify the primary care provider who may order diagnostic tests, a dietary consultation, and changes in the type of diet. This measure is not adjusted for resident characteristics.
Percentage of long-stay residents with new or worsened bowel or bladder incontinence. (Data source: CMS MDS Quality Measures, 10/01/2023 – 09/30/2024)
This measure reports the percent of long-stay residents with new or worsened ability to control their bowels or bladder. Over half of nursing home residents are incontinent of urine, which can increase their risk for falls with injury and pressure ulcers/injuries. Residents who are incontinent often avoid group activities due to embarrassment and may have a lower quality of life. Staff can reduce incontinence episodes by employing strategies such as bladder or bowel training and prompted or scheduled voiding. This measure is not adjusted for resident characteristics.
Health and Safety Inspections?
| Current | State Average | |
|---|---|---|
Combined Federal and State Health Inspections Rating |  (higher is better) (higher is better) |
NA |
Federal fines issued for violations from the last three years ($) | $0 (lower is better) |
$29,745 (lower is better) |
Total federal and state fines ($) | $0 (lower is better) |
$62,496 (lower is better) |
Number of days the facility was denied payment due to unresolved violations | 0 (lower is better) |
0.0 (lower is better) |
Health and Safety Inspections
Combined Federal and State Health Inspections Rating (Data Source: Cal Long Term Care Compare: 10/1/2022 through 9/30/2025)
This rating is based on the number and type of state and federal citations that were found during the reporting period. More weight is given to the most recent health inspection and, therefore, the most recent violations. The state may cite a facility for the same violation that the federal government identifies, while other times the federal and state violations are completely different.
Federal fines issued for violations from the last three years ($) (Data Source: CMS Penalties: through 9/30/2025)
This figure shows the total dollar amount in fines that CMS has charged the nursing home for not following health and safety rules during the specified period. The amount of the fines can vary depending on how many residents were affected or the seriousness of the violation. Most nursing homes do not have any federal fines.
Total federal and state fines ($) (Data Source: CMS Penalties; CA Health Facilities State Enforcement Actions: through 9/30/2025)
This is the total dollar amount charged to the nursing home for not following federal and/or state health and safety rules. Most nursing homes do not have any federal or state fines.
Number of days the facility was denied payment due to unresolved violations (Data Source: CMS Penalties: through 9/30/2025)
This is the number of days the nursing home could not receive Medicare payments for new residents because of unresolved violations. Most nursing homes do not have any denials of payment.
Facility Description?
| Current | State Average | |
|---|---|---|
Special Focus Facility | No |
NA |
Facility type | Freestanding |
NA |
Resident population | Adult |
NA |
Payments accepted | Medicare and Medicaid |
NA |
Number of beds | 128 |
97.0 |
Type of Specialty Care Available |
||
Subacute beds | Yes |
NA |
Ventilator beds | Contact facility |
NA |
Alzheimer's/dementia program | No |
NA |
Hospice program | Contact facility |
NA |
Long-term rehabilitation | Contact facility |
NA |
Behavioral health/psychiatric | No |
NA |
Continuing care retirement community | No |
NA |
Resident council | Yes |
NA |
Family council | No |
NA |
Facility Description
The Facility Description section includes some of the information found in the At-A-Glance section as well as additional information on the types of care available in nursing homes.
Special Focus Facility (Data Source: CMS Provider Data: through 9/30/2025)
The U.S. Centers for Medicare & Medicaid Services (CMS) created the Special Focus Facility (SFF) initiative to stimulate systematic improvements in quality of care. CMS has found that a small number of nursing homes have more serious problems than most other nursing homes or problems that have persisted for at least three years. CMS requires that SFF nursing homes be visited in person by survey teams twice as frequently as other nursing homes to ensure improvements are being made. CMS limits California to 6 nursing homes on the SFF list at one time. For more information, see the CMS website.
Facility type (Data Source: CMS Provider Data; CDPH Licensed and Certified Healthcare Facility Listing: through 9/30/2025)
There are two basic types of skilled nursing facilities: freestanding or a distinct part of a hospital.
- Freestanding: Freestanding facilities provide 24-hour skilled nursing care to assist with short term recovery from a surgery, injury, or acute illness or provide on-going nursing home care for those who need more permanent long-term care.
- Distinct Part of acute care hospital: A Distinct Part facility is always associated with a hospital. It must be physically distinguishable from the hospital (separate address) and fiscally separate for cost reporting purposes. A Distinct Part facility provides the same services as a freestanding facility as well as treatment for acute illness or injury and intensive rehabilitation services. Most residents stay a brief time, usually a maximum of three weeks, and then are discharged to either a freestanding nursing home or back to their own home.
Resident population (Data Source: CMS Provider Data; CDPH Licensed and Certified Healthcare Facility Listing: through 9/30/2025)
A nursing home may serve only adults, only children (pediatric) or both adults and children.
Payments accepted (Data Source: CDPH Licensed and Certified Healthcare Facility Listing: through 9/30/2025)
All nursing homes in California accept insurance payments directly from insurance companies (including private insurance and long-term care insurance). In addition, many are certified to receive payment from the Medicare program for short term stays defined as the first 100 days (about 3 and a half months) of care. Medicare pays most costs (excluding co-pays) for those who are Medicare beneficiaries. Medicare does not pay for stays beyond 100 consecutive days, at which point residents are considered to be long-term care residents. Some, but not all, facilities accept payment from the Medicaid program (Medi-Cal) for long-term residents with low incomes and few assets. If the resident does not qualify for Medi-Cal, they will be billed for the cost of care.
Number of beds (Data Source: CDPH Licensed and Certified Healthcare Facility Listing: through 9/30/2025)
This indicates the number of licensed beds distributed among private and shared rooms that have been certified to be paid for by Medicare and/or Medi-Cal.
Type of Specialty Care Available
- Subacute Care (Data Source: CDPH Licensed and Certified Healthcare Facility Listing, 03/17/2025): More intense care than skilled nursing care, but less intense than acute hospital care. It involves intensive nursing and supportive and therapeutic care provided by licensed nurses for residents with fragile medical conditions.
- Ventilator Beds (Data Source: LTC (Long Term Care) Facility Integrated Disclosure and Medi-Cal Cost Report Data 12/31/2023): Ventilators or respirators are machines that mechanically assist patients with breathing and are sometimes referred to as artificial respiration. Ventilator beds are part of a subacute nursing home.
- Alzheimer’s/Dementia Program (Data Source: HCAI Long-Term Care Facilities Annual Utilization Report 12/31/2023): Almost all nursing homes will accept residents with cognitive impairment, including Alzheimer’s disease. However, there are nursing homes that specialize only in dementia care and others that may have a designated memory care unit.
- Hospice Program (Data Source: HCAI Long-Term Care Facilities Annual Utilization Report 12/31/2023): Hospice provides additional services from a team that specializes in end-of-life care. Hospice provides comprehensive comfort care including pain management as well as counseling services for residents and their families. Most nursing homes contract with an outside certified Hospice Provider.
- Long-term Rehabilitation (Data Source: HCAI Long-Term Care Facilities Annual Utilization Report 12/31/2023): Intensive rehabilitation services (such as intensive physical and occupational therapy) are designed to make a patient as independent as possible after a prolonged illness or major injury.
- Behavioral health/psychiatric (Data Source: CDPH Licensed and Certified Healthcare Facility Listing, 03/17/2025): In California, Behavioral Health facilities, also called Psychiatric Health Facilities, provide 24-hour inpatient care for people requiring skilled nursing who meet legal definitions of mental disorder or incompetence. Specialty care includes, but is not limited to psychiatry, clinical psychology, psychiatric nursing, social work, rehabilitation, and drug administration.
- Continuing Care Retirement Community (Data Source: CMS Provider Data; CDPH Licensed and Certified Healthcare Facility Listing 03/17/2025): Some nursing homes may be part of a continuing care retirement community (CCRC). A CCRC provides a continuum of services, including independent living, assisted living, and skilled nursing home care on a single campus. Residents can move between levels of care based on their changing needs.
Resident or family councils (Data Source: CMS Provider Data, 03/17/2025):
A resident council is an organized group of nursing home residents, supported by the nursing home administration, who meet regularly to improve the quality of care and quality of life in the facility and to promote and protect residents’ rights. California and federal law ensures the right of residents to organize and participate in a resident council. Family councils are optional, but are a similar facility supported organization that includes family members. This measure does not reflect how often the councils meet or the extent of involvement of residents and/or families.
Staffing?
| Current | State Average | |
|---|---|---|
CLTCC Staffing Rating |  (higher is better) (higher is better) |
NA |
Staffing
CLTCC Staffing Rating (Data Source: Cal Long Term Care Compare: 1/1/2025 through 3/31/2025)
Most nursing homes in California care for a combination of people who are either recovering from a hospital stay or need long-term care. Evidence shows that staffing levels in nursing homes can affect the quality of care that residents receive in the nursing home. The CLTCC Staffing Rating shows whether the nursing home meets California’s minimum nurse staff hour requirements and whether it also provides enough hours of nursing care to meet the needs of its residents based on their severity of illness.
California Minimum Requirements: California law requires its nursing homes to provide at least 3.5 hours of direct nursing care per resident day, with at least 2.4 hours of that time coming from certified nursing assistants (CNAs). This does not mean that each resident gets 3.5 hours of nursing care every day because residents who are sicker or require complex care will need more hours of care per day while healthier residents will need less nursing care.
Expected Nursing Hours: The best nursing homes not only meet the state’s minimum requirement, but they also increase their staff hours based on the health conditions or severity of illness of their residents. The CLTCC rating includes the number of staff needed based on the severity of all residents in the nursing home during the measurement period. This calculation can help nursing homes estimate the expected nursing hours needed to care for all their residents’ needs. The number of hours may exceed California’s minimum staffing requirement.
Nursing homes that meet minimum nursing hour requirements and meet or go beyond expected nursing hours get higher ratings.
Rating definitions:
- Poor: Did not provide California’s minimum nurse staff hours requirement. Specifically – failed to meet the California minimum requirement for both CNAs and total nurse staffing.
- Below Average: Met only part of the state requirement. Specifically – met only ONE of the two state minimum staffing requirements, either CNA or total nurse staffing.
- Average: Met or exceeded the California minimum staffing hours, but did not meet the expected hours for either CNA hours or total nursing hours based on residents’ severity of illness.
- Above Average: Had enough staff to meet California’s minimum nurse staff hours requirement and met or exceeded expectations for either CNA hours or total staffing hours based on residents’ severity of illness.
- Superior: Met the state minimum requirements and met or exceeded expected hours for both CNA and total nurse staff hours based on residents’ severity of illness.
Nursing retention and turnover?
| Current | State Average | |
|---|---|---|
Percent of nursing staff who worked in the facility continuously for 12 months | 89% (higher is better) |
70.0% (higher is better) |
Nursing staff turnover | 40% (lower is better) |
39.0% (lower is better) |
Number of administrators who have left the nursing home in the past 12 months | 0.0 (lower is better) |
0.0 (lower is better) |
Nursing retention and turnover
Nursing staff retention (when staff remain employed with the organization all year) and turnover (when staff leave the organization during the year) are frequently related. Lower staff retention rates are usually associated with high rates of staff turnover. Occasionally, a nursing home may have both high nursing staff retention and high turnover meaning that most staff stayed all year, but a smaller number of positions had a lot of staff joining and leaving the facility during the year. This pattern may result from the management of the facility or a change in the type or number of patients, or a change in the number of staffed beds.
Percent of nursing staff who worked in the facility continuously for 12 months (Data Source: LTC Facility Integrated Disclosure and Medi-Cal Cost Report Data: 1/1/2023 through 12/31/2023)
This measure reflects the percentage of all nursing staff (registered nurses, licensed practical/vocational nurses, and certified nursing assistants) who stayed in their job for the past 12 months (rate of retention). Nursing staff who remain in the nursing home are generally more satisfied with their jobs. Higher retention rates can be associated with higher quality of care because there is more stability among the nursing home workforce. If a nursing home has low staff retention, families should ask about the reasons and how it affects care.
Nursing staff turnover (Data Source: CMS Provider Data: 1/1/2024 through 12/31/2024)
The turnover measure shows the percent of all nursing staff (registered nurses, licensed practical/vocational nurses, and certified nursing assistants) who stopped working at the nursing home over a 12-month period. When nursing staff is constantly changing, it may be stressful and disruptive for residents to receive care from new staff who are unfamiliar with their routines or special needs. Evidence shows that the lower the nursing staff turnover rate at a nursing facility, the better the quality, continuity, and stability of care. If a nursing home has high turnover, families should ask about the reasons and how it affects care.
Number of administrators who have left the nursing home in the past 12 months (Data Source: CMS Provider Data: 1/1/2024 through 12/31/2024)
This measure shows how many administrators (the people who manage the nursing home) left their jobs over a year. Each nursing home needs a licensed administrator to run things smoothly and help improve the quality of care. Frequent changes in this position can affect how well the facility is managed.
Quality of Care?
| Current | |
|---|---|
CMS 5-Star rating for short stay |  |
CMS 5-Star rating for long stay |  |
Quality of Care
Overall Quality Measures
This section provides details about measures that can inform residents, their families, and others about the quality of care in nursing homes (also called skilled nursing facilities [SNF]) and how the quality is measured. In general, nursing homes should ensure that they are working with residents and families to address the residents’ goals of care. They should also have systems in place to prevent harm (e.g., falls, pressure injuries, infections) to residents and have a process for ongoing quality improvement.
Patients who are newly admitted to the nursing home from the hospital and are receiving rehabilitation services and/or intensive nursing care are usually considered short-stay residents. While they may have up to 100 days paid by Medicare, the average patient spends a few weeks in the nursing home for rehabilitation and then finishes their rehabilitation at home. When short-stay residents have achieved their short-stay goals or are no longer making any progress in their rehabilitation, they no longer qualify for Medicare coverage, at which point they are discharged home or transitioned to long-stay.
The ultimate goal for short-stay residents is to be discharged back to their homes to live independently; improving and sustaining gains in their function and ability to care for themselves should be high priorities for the nursing home to support.
Long-stay residents are in the nursing home either as a direct-admission from home without a qualifying hospital admission; as short-stay residents who convert to long-stay because they are no longer making progress in rehabilitation; or because they reached the Medicare 100-day maximum coverage. Patients who are not Medicare beneficiaries can also be admitted to the nursing home from the hospital or home – the rules for those residents depend on their insurance status. These services can be paid for through Medi-Cal, long term care insurance, or residents paying out of pocket.
The goals for long-stay residents are to maintain the highest functional ability possible or at least to slow the loss of functional abilities and to maintain the best possible quality of life.
CMS 5-Star rating for short stay (Data Source: CMS Provider Data: through 9/30/2025)
The US Centers for Medicare & Medicaid Services (CMS) created a five-star quality rating system to help consumers, their families, and caregivers compare nursing homes more easily and to help identify areas about which you may want to ask questions. Nursing homes with five stars are considered to have above average quality, and nursing homes with one star are considered to have below average quality. For more information, see the CMS website. This rating is a composite rating of six select short-stay measures:
Derived from Claims-Billing Data:
- Percentage of short-stay residents who were re-hospitalized after a nursing home admission
- Percentage of short-stay residents who have had an outpatient emergency department visit
- Rate of successful return to home and community from a SNF
Derived from Nursing Assessment:
- Percentage of short-stay residents who got antipsychotic medication for the first time
- Percentage of short-stay residents who improved in their ability to move around on their own
- Percentage of residents with pressure ulcers/pressure injuries that are new or worsened
CMS 5-Star rating for long stay (Data Source: CMS Provider Data: through 9/30/2025)
The US Centers for Medicare & Medicaid Services (CMS) created a five-star quality rating system to help consumers, their families, and caregivers compare nursing homes more easily and to help identify areas about which you may want to ask questions. Nursing homes with five stars are considered to have above average quality, and nursing homes with one star are considered to have below average quality. For more information, see the CMS website. This rating is a composite rating of nine select long-stay measures:
Derived from Claims-Billing Data:
- Number of hospitalizations per 1,000 long-stay resident days
- Number of outpatient emergency department visits per 1,000 long-stay resident days
Derived from the Nursing Assessment
- Percentage of long-stay residents who got an antipsychotic medication
- Percentage of long-stay residents experiencing one or more falls with major injury
- Percentage of long-stay residents with pressure ulcers
- Percentage of long-stay residents with a urinary tract infection
- Percentage of long-stay residents who have or had a catheter inserted and left in their bladder
- Percentage of long-stay residents whose ability to walk independently worsened
- Percentage of long-stay residents whose need for help with activities of daily living increased
Vaccinations?
| Current | State Average | |
|---|---|---|
Influenza Vaccination |
||
Percentage of short-stay residents who were assessed and appropriately given the seasonal influenza vaccine | 100% (higher is better) |
93.0% (higher is better) |
Percentage of long-stay residents assessed and appropriately given the seasonal influenza vaccine | 100% (higher is better) |
98.0% (higher is better) |
Pneumonia Vaccination |
||
Percentage of short-stay residents assessed and appropriately given the pneumococcal vaccine | 100% (higher is better) |
93.0% (higher is better) |
Percentage of long-stay residents assessed and appropriately given the pneumococcal vaccine | 100% (higher is better) |
98.0% (higher is better) |
Vaccinations
Older adult residents are particularly vulnerable to influenza (flu) and pneumonia. Vaccines are important tools for preventing serious disease and death. This section reports vaccination rates for two types of infection: influenza (flu) and pneumonia
Residents are excluded if they have an allergy to the vaccine; have an order not to immunize or a history of Guillain-Barre Syndrome; are moderately to severely ill; or have a weakened immune system.
Influenza Vaccination (Data Source: CMS MDS Quality Measures: 7/1/2023 through 6/30/2024)
The Centers for Disease Control and Prevention (CDC) require that influenza (flu) vaccinations be offered to residents and staff to prevent the spread of flu in nursing homes. The staff flu vaccination rate data are not publicly available, so we are unable to report it here; however, residents and families may want to ask the nursing home about their staff flu vaccination rates.
These measures report the percentage of short-stay and long-stay residents who were: given, and appropriately received, the influenza vaccine during the most recent flu season.
Pneumonia Vaccination (Data Source: CMS MDS Quality Measures: 1/1/2024 through 3/31/2025)
Pneumonia vaccines are strongly recommended for children with certain medical conditions and for most adults aged 65 years or older who have a healthy immune system. Like the flu vaccine, pneumonia vaccines also are required to be offered to all nursing home residents who are eligible.
Pneumonia is a significant cause of death from a bacterial disease in older adults. These measures report the percentage of short-stay and long-stay residents aged 65 or older who have an up-to-date pneumonia vaccine during the reporting period.
Short Stay Resident Health and Safety?
| Current | State Average | |
|---|---|---|
Rehospitalizations and Emergency Department Visits |
||
Percentage of short-stay residents who were re-hospitalized after a nursing home admission | 19% (lower is better) |
22.0% (lower is better) |
Rate of potentially preventable hospital readmissions 30 days after discharge from a SNF | 14% (lower is better) |
11.0% (lower is better) |
Percentage of short-stay residents who have had an outpatient emergency department visit | 10% (lower is better) |
11.0% (lower is better) |
Medications |
||
Percentage of short-stay residents who got antipsychotic medication for the first time | 1.0% (lower is better) |
1.4% (lower is better) |
Percentage of residents whose medications were reviewed and who received follow-up care when medication issues were identified | 100% (higher is better) |
93.0% (higher is better) |
Resident Safety |
||
Percentage of residents with pressure ulcers/pressure injuries that are new or worsened | 0.0% (lower is better) |
1.2% (lower is better) |
Percentage of SNF residents who experience one or more falls with major injury during their SNF stay | 0.0% (lower is better) |
0.4% (lower is better) |
Rate of healthcare associated infections acquired during the SNF stay that resulted in hospitalization | 7% (higher is better) |
8.0% (higher is better) |
Resident Change in Ability and Mobility |
||
Rate of successful return to home and community from a nursing home | 56% (higher is better) |
51.0% (higher is better) |
Percentage of residents who are at or above an expected ability to care for themselves and move around at discharge | 54% (higher is better) |
51.0% (higher is better) |
Percentage of residents who are at or above an expected ability to move around at discharge | 57% (higher is better) |
48.0% (higher is better) |
Percentage of residents who are at or above an expected ability to care for themselves at discharge | 61% (higher is better) |
51.0% (higher is better) |
Short Stay Resident Health and Safety
The short-stay measures section includes assessment and outcome measures for short-stay residents, who may stay in a nursing home (also called a skilled nursing facility [SNF]) for up to 100 days after acute hospitalization for the purpose of rehabilitation and goal of returning to their previous home setting. Each of these measures may have some residents who are excluded; for example, they are enrolled in hospice or have serious brain injuries.
Rehospitalizations and Emergency Department Visits
- Percentage of short-stay residents who were re-hospitalized after a nursing home admission (Data source: CMS Medicare Claims Quality Measures, 01/01/2024 – 12/31/24)
The measure reports the percentage of short-stay residents who initially entered the nursing home from a hospital and were then re-admitted to a hospital for an unplanned inpatient or observation stay within 30 days of the start of the nursing home stay for any condition that could have been prevented. This CMS measure adjusts for resident characteristics such as age, prior functional status, complexity of medical conditions, and co-occurring illnesses. Nursing homes should ensure that short-stay residents can be safely discharged home in a stable condition. High rates of hospital readmissions may indicate that the nursing home did not prevent complications when caring for the resident.
- Rate of potentially preventable hospital readmissions 30 days after discharge from a SNF (Data source: CMS SNF Quality Reporting Program-Provider Data,10/1/2021 – 09/30/2023)
This measure looks at how many short-stay residents go back to the hospital within 30 days after leaving the nursing home. It checks if the hospital visit could have been prevented. The measure considers characteristics like the residents’ age, how they were doing before hospitalization, and other health issues. Some residents, like those who planned to go back to the hospital, are not counted. Hospital readmissions place residents at greater risk of infections, falls, and pressure injuries, are costly, and are often avoidable. Nursing homes should ensure that residents are medically stable and ready for safe discharge and should teach residents and families about the residents’ medications, treatments, and conditions to monitor. Most residents will qualify for a home health visit after a SNF discharge, which may also help prevent rehospitalization. Better staffing has been shown to decrease the rate of potentially avoidable readmissions.
- Percentage of short-stay residents who have had an outpatient emergency department visit (Data source: CMS Medicare Claims Quality Measures, 01/01/2024 – 12/31/2024)
This measure reports the percentage of short-stay residents who entered the nursing home from a hospital and were sent to an emergency department within 30 days of the start of the nursing home stay, but in which the ED visit did not result in an inpatient or observation stay. High rates of ED visits may indicate that the nursing home is not providing adequate care. Nursing homes must assess short-stay residents frequently for subtle signs that their condition is getting worse, notify their primary care provider about early changes of condition, and implement appropriate treatments. This measure is adjusted to be more fair among nursing homes because it takes into account characteristics about each resident like their age and how sick they are.
Medications
- Percentage of short-stay residents who got antipsychotic medication for the first time (Data source: CMS MDS Quality Measures, 01/01/2024 – 03/31/2025)
Antipsychotic medications are used to treat a very specific group of mental health conditions such as schizophrenia; however, these drugs historically were used to manage agitated behaviors in residents without schizophrenia or other appropriate medical conditions. This measure reports the percentage of short-stay residents who received an antipsychotic for the first time in the nursing home. This class of medications can cause serious harm and should not be given to control mood or behavior, particularly in residents with dementia. Some residents were excluded from this measure such as those already on an antipsychotic at admission or who have a diagnosis of schizophrenia, Tourette’s syndrome, or Huntington’s disease, for which antipsychotics are appropriate. High rates of antipsychotic use may indicate poor quality of care. Nursing homes should use alternative methods to reduce agitation such as increased exercise, improved pain management, music therapy, and other non-drug interventions. This measure is not adjusted for resident characteristics.
- Percentage of short-stay residents whose medications were reviewed and who received follow-up care when medication issues were identified (Data source CMS SNF Quality Reporting Program-Provider Data, 10/01/2023 – 09/30/2024)
When residents transfer from the hospital to the nursing home, there is an increased risk for medical errors particularly in the type of medications that are to be stopped from the hospital and ones that need to be started in the nursing home. This measure reports the percentage of short-stay residents who had a medication review at admission that showed significant problems with medications and had a timely follow-up with a clinician to address the problems. Resident conditions may change rapidly during the post-hospitalization stay in the nursing home and may require frequent changes in medications. Nursing homes should ensure that primary care providers are notified promptly of changes in condition and that timely medication changes, if ordered, are implemented. This measure is not adjusted for resident characteristics.
Resident Safety
- Percentage of residents with pressure ulcers/pressure injuries that are new or worsened (Data Source: CMS SNF Quality Reporting Program- Provider Data: 10/01/2023 – 09/30/2024)
This measure reports the percentage of residents who develop new or worsening Stage II-IV pressure ulcers (also known as pressure sores or injuries). Pressure ulcers are areas of damaged skin caused by the resident staying in one position for too long; prolonged pressure in that area causes breakdown in the skin and underlying tissue resulting in a pressure sore. Residents who develop new pressure ulcers/injuries are likely not being turned and repositioned properly or frequently enough, which can result in serious consequences including pain, infection, and death. If the resident cannot turn independently, nursing home staff should turn and reposition residents frequently (usually every 2 hours), keep their skin dry, use appropriate support surfaces (e.g., special beds), and minimize injury from medical devices that cause pressure on the skin. This measure is adjusted to be more fair among nursing homes because it takes into account characteristics about each resident like their age and how sick they are.
- Percentage of short-stay residents who experience one or more falls with major injury during their SNF stay (Data Source: CMS SNF Quality Reporting Program – Provider Data, 10/01/2023 – 09/30/2024)
Falls with a major injury are considered a “never event” (because they should never happen) and may reflect lower quality of care. This measure reflects the percentage of short-stay residents who experience one or more falls associated with a major injury such as a fracture, loss of consciousness, or head injury while in the nursing home. Risk of falls must be balanced with the importance of resident mobility, so the key is to prevent injury if there is a fall. Nursing homes should have some type of fall prevention program in place to help prevent major injuries from falls. This measure is not adjusted for resident characteristics.
- Percentage of infections patients got during their SNF stay that resulted in hospitalization (Data source CMS SNF Quality Reporting Program-Provider Data, 10/01/2022 – 09/30/2023)
Healthcare-associated infections (HAIs) are infections that patients can get while receiving care in a SNF. These infections are usually the result of a lack of prevention strategies like hand washing and using personal protective equipment. This measure shows the rate of healthcare-associated infections that patients get during their SNF stay that result in hospitalization. This measure includes infections developed starting on day 4 of the nursing home stay and within 3 days after discharge.
Resident Change in Ability and Mobility
- Percentage of successful return to home and community from a nursing home (Data source: CMS SNF Quality Reporting Program-Provider Data, 10/01/2021 – 09/30/2023)
This measure reports the percentage of short-stay residents admitted to the nursing home from a hospital who were then discharged to the community within 100 calendar days of admission, and who remained in the community for at least 30 consecutive days following discharge to the community. This measure is adjusted to be more fair among nursing homes because it takes into account characteristics about each resident like their age and how sick they are. If nursing homes have high numbers of residents who are readmitted to the hospital after discharge, it may indicate they are not adequately preparing residents for discharge or appropriately evaluating residents’ readiness to successfully care for themselves at home.
- Percentage of residents who are at or above an expected ability to care for themselves and move around at discharge. (Data source: CMS SNF Quality Reporting Program-Provider Data, 10/01/2023 – 09/30/2024)
This measure reports the percentage of residents who are at or above their expected ability to care for themselves and move around when discharged from the SNF. Reducing difficulties with activities like eating, toileting, and moving around can improve residents’ quality of life. This measure is adjusted to be more fair among nursing homes because it takes into account characteristics about each resident like their age and how sick they are.
- Percentage of residents who are at or above an expected ability to move around at discharge (Data source CMS SNF Quality Reporting Program-Provider Data, 10/01/2023 – 09/30/2024)
This measure estimates the percentage of short-stay residents with a mobility score at or above the discharge score that was expected for them. The scores range from 15-90 and are risk-adjusted based on resident characteristics such as age, prior functional status, and complexity of medical conditions. Mobility items include activities such as the ability roll from side to side, change positions from lying to sitting to standing, move from bed to chair or toilet, and walk or climb stairs.
- Percentage of residents who are at or above an expected ability to care for themselves at discharge (Data source CMS SNF Quality Reporting Program-Provider Data, 10/01/2023 – 09/30/2024)
This measure estimates the percentage of short-stay residents who meet or exceed the expected self-care score at discharge. It is important that nursing homes prepare residents to care for themselves when they are discharged home. Scores range from 7-42 and are risk-adjusted based on resident age, prior functioning, and medical conditions. Self-care activities, such as eating, oral hygiene, toileting, bathing, upper and lower body dressing, are evaluated using a 6-point scale for each item.
Long Stay Resident Health and Safety?
| Current | State Average | |
|---|---|---|
Hospitalizations and Emergency Department Visits |
||
Number of hospitalizations per 1,000 long-stay resident days | 2.0 (lower is better) |
2.2 (lower is better) |
Number of outpatient emergency department visits per 1,000 long-stay resident days | 2.3 (lower is better) |
1.6 (lower is better) |
Medications |
||
Percentage of long-stay residents who received an antipsychotic medication | 2% (lower is better) |
10.0% (lower is better) |
Percentage of long-stay residents who got an antianxiety or hypnotic medication | 21% (lower is better) |
14.0% (lower is better) |
Resident Safety |
||
Percentage of long-stay residents experiencing one or more falls with major injury | 1.0% (lower is better) |
1.7% (lower is better) |
Percentage of long-stay residents with pressure ulcers | 6% (lower is better) |
5.0% (lower is better) |
Percentage of long-stay residents who were physically restrained | 0.0% (lower is better) |
0.4% (lower is better) |
Resident Change in Ability and Mobility |
||
Percentage of long-stay residents whose ability to walk independently worsened | 4% (lower is better) |
13.0% (lower is better) |
Percentage of long-stay residents whose need for help with activities of daily living increased | 5% (lower is better) |
12.0% (lower is better) |
Health Care Quality |
||
Percentage of long-stay residents who have symptoms of depression | 2% (lower is better) |
6.0% (lower is better) |
Percentage of long-stay residents who lose too much weight | 3% (lower is better) |
4.3% (lower is better) |
Percentage of long-stay residents with a urinary tract infection | 0.0% (lower is better) |
1.3% (lower is better) |
Percentage of long-stay residents who have or had a catheter inserted and left in their bladder | 0.0% (lower is better) |
1.2% (lower is better) |
Percentage of long-stay residents with new or worsened bowel or bladder incontinence | 2% (lower is better) |
12.0% (lower is better) |
Long Stay Resident Health and Safety
The measures in this section apply to residents who reside in the nursing home (also called a skilled nursing facility [SNF]) for an extended period of time. For residents who were admitted from an acute care hospital to the nursing home, it is the date when the resident no longer qualifies for short stay rehabilitation. In any case, Medicare only covers the first 100 days of a SNF admission. These residents may stay in the nursing home for months, years, or the rest of their lives. In general, the goals of long-term care are to maintain physical and mental function, prevent harm, and provide an environment to enhance the quality of life for residents. The care should be focused on the individual resident and family goals for care.
There are general exclusions in some of these measures for residents who are in hospice care, or who are comatose or paralyzed, or who have severe brain injuries. Other measure-specific exclusions are described below.
Hospitalizations and Emergency Department Visits (Data Source: CMS Medicare Claims Quality Measures: 1/1/2024 through 12/31/2024)
- Number of hospitalizations per 1,000 long-stay resident days
This measure reports the number of unplanned inpatient admissions or outpatient observation stays at an acute care or critical access hospital that occurred in the target period while the individual was a long-term care nursing home resident. Residents with a planned hospital inpatient admission, who were not a Medicare beneficiary, or were in hospice are excluded. This measure is adjusted to be more fair among nursing homes because it takes into account characteristics about each resident like their age and how sick they are.
- Number of outpatient emergency department visits per 1,000 long-stay resident days
This measure represents the number of unplanned outpatient emergency department visits for any reason that do not result in an outpatient observation or inpatient hospital stay and that occurred in the target period while the individual was a long-term care nursing home resident. Residents who were not a Medicare beneficiary or were on hospice are excluded. This measure is adjusted to be more fair among nursing homes because it takes into account characteristics about each resident like their age and how sick they are.
Medications (Data Source: CMS MDS Quality Measures: 4/1/2024 through 3/31/2025)
- Percentage of long-stay residents who received an antipsychotic medication
Antipsychotic medications are used to treat a very specific group of mental health conditions such as schizophrenia; however, these drugs historically have been used to manage agitated behaviors in residents without schizophrenia or other appropriate medical conditions. This measure reports the percentage of long-stay residents who received an antipsychotic medication during the reporting period. This class of medications can cause serious harm and should not be given to control mood or behavior, particularly in residents with dementia. Those who have a diagnosis of schizophrenia, Tourette’s syndrome, or Huntington’s disease were excluded from this measure as antipsychotics are appropriate for these residents. Nursing homes should employ alternative methods to reduce agitation such as increased exercise, improved pain management, music therapy, and other non-drug interventions. High rates of antipsychotic use may indicate poor quality of care. Nursing homes should have non-pharmacological programs to manage resident behavioral issues. This measure is not adjusted for resident characteristics.
- Percentage of long-stay residents who got an antianxiety or hypnotic medication
This measure shows how many long-stay residents took medication for anxiety or to help them sleep during the reporting period. Residents were excluded if they were in hospice care where these medications may be helpful. Nursing homes should look for underlying causes of resident anxiety or inability to sleep prior to use of medications because both classes of medications may have serious side effects such as excessive sleepiness. These side effects could lead to falls with injury and pressure ulcers among other problems. This measure is not adjusted for resident characteristics.
Resident Safety (Data Source: CMS MDS Quality Measures: 4/1/2024 through 3/31/2025)
- Percentage of long-stay residents experiencing one or more falls with major injury
Falls with a major injury are considered a “never event” (because they should never happen) and may reflect lower quality of care. This measure reports the percentage of resident stays during which one or more falls with a major injury (bone fracture, joint dislocation, closed head injury with altered consciousness, or subdural hematoma) occurred. Falls must be balanced with the importance of resident mobility, so the key is to prevent injury if there is a fall. Nursing homes should have some type of prevention program in place to help prevent major injuries from falls. This measure is not adjusted for resident characteristics.
- Percentage of long-stay residents with pressure ulcers
Pressure ulcers (also known as pressure injuries or sores) are areas of damaged skin caused by the resident staying in one position for too long; prolonged pressure in that area causes breakdown in the skin and underlying tissue resulting in a pressure sore, ulcer or open wound. Long-stay residents who have at least one of the following conditions are considered to be at high-risk for pressure ulcers: impaired mobility (difficulty moving), difficulty staying nourished (poor nutrition), or in a coma. This measure reports high-risk, long-stay residents who have pressure ulcers/injuries. These residents are dependent upon the nursing staff to turn and reposition them frequently to avoid pressure ulcers/injuries. Nursing homes should have a strong pressure ulcer/injury program that emphasizes frequent repositioning in residents at high risk. This measure is not adjusted for resident characteristics.
- Percentage of long-stay residents who were physically restrained
The measure reflects the percentage of long-stay residents who were physically restrained on a daily basis during the reporting period. Restraints are defined as any manual, physical, or mechanical device, material or equipment that prevents or restricts the resident from being mobile. Examples include vests, straps or belts, limb ties, wheelchair trays or bars that cannot be removed by the resident, as well as bed siderails, particularly siderails that extend the full length of the bed. Physical restraints have been known to cause significant injury and death and should rarely be used. Nursing homes should ensure that residents with any type of restraint always be able to be directly observed by staff for safety reasons. Alternative options for restraints may include lowering the bed and placing a floor pad next to it to protect the patient if they roll off the bed or fall when getting up. This provides a safer environment that allows a resident more freedom. This measure is not adjusted for resident characteristics.
Resident Change in Ability and Mobility (Data Source: CMS MDS Quality Measures: 4/1/2024 through 3/31/2025)
- Percentage of long-stay residents whose ability to walk independently worsened
This measure reports the percent of long-stay residents who experienced a decline in independence of locomotion (bed mobility, transferring, or walking) during the target period. Residents are excluded from this measure if they are comatose, in hospice or with prognosis of < 6 months to live or were totally dependent on previous assessments. Nursing home staff should provide restorative care or physical therapy to prevent these losses when possible. This measure is adjusted to be more fair among nursing homes because it takes into account characteristics about each resident like their age and how sick they are.
- Percentage of long-stay residents whose need for help with activities of daily living increased
This measure reports the percentage of long-stay residents who have an increased need for help with activities of daily living (ADLs) since the last assessment. It measures four specific activities thought to be lost only late in life: bed mobility, bed transfers, eating, and toileting. Residents are excluded if they were totally dependent for all four activities or 3 of 4 activities in prior assessments, are comatose, have a life expectancy < 6 months, or are on hospice. While some loss of these functions might be expected in some residents, nursing homes with very high scores may indicate poor quality of care. Nursing home staff should provide restorative care or occupational or physical therapy to prevent these losses when possible. This measure is not adjusted for resident characteristics.
Health Care Quality (Data Source: CMS MDS Quality Measures: 4/1/2024 through 3/31/2025)
- Percentage of long-stay residents who have symptoms of depression
This measure reflects the percent of long-stay residents who have had symptoms of depression. The symptoms are measured by loss of interest or pleasure, feeling down, depressed, or hopeless either verbally expressed in an interview or observed by staff. Residents who are comatose are excluded. Depression is not uncommon in older adults and may reflect a poor quality of life. Some residents may need medications, which must be ordered by their primary care or psychiatric care provider. However, caution should be taken as some medications may increase risk for falls or have serious side effects. Nursing homes should engage residents in meaningful ways with individual and group activities such as music therapy, socialization with friends and family, and efforts to improve their mobility and participation in activities of daily living to prevent or reduce symptoms of depression. This measure is not adjusted for resident characteristics.
- Percentage of long-stay residents who lose too much weight
Unexpected or unintentional weight loss is often associated with poor health outcomes and could be associated with an underlying illness. However, it may also be associated with certain medications, difficulty chewing or swallowing food, poor dental health, and depression among other causes. Nursing home staff should monitor each resident’s weight regularly and if there is unintentional, significant weight loss (5% or more in the last month or 10% or more in the last 6 months), they should notify the primary care provider who may order diagnostic tests, a dietary consultation, and changes in the type of diet. This measure is not adjusted for resident characteristics.
- Percentage of long-stay residents with a urinary tract infection
This measure reports the percentage of long-stay residents who have had a urinary tract infection (UTI) within a 30-day period, where the resident has positive signs or symptoms and laboratory findings requiring medication. UTIs are common in nursing homes and may be prevented with proper hydration, nutrition, mobility, improved voiding habits, and better perineal hygiene. Higher numbers of residents with UTIs may indicate poor care. Nursing homes should use regular hydration processes and prompted or scheduled voiding processes, which may reduce the incidence of UTIs. This measure is not adjusted for resident characteristics.
- Percentage of long-stay residents who have or had a catheter inserted and left in their bladder
A catheter is a tube placed in the body to drain and collect urine from the bladder, which may be necessary for residents who have lost bladder function. This measure reports the number of residents who have a catheter left in their bladder during a 7-day reporting period. Residents with neurogenic bladder (the bladder is damaged due to a central nervous system disease or injury and does not empty normally) or obstruction in the urine system are excluded from this measure because an indwelling catheter (left in place) is necessary. Residents with indwelling catheters are at high risk for bladder infections. One alternative is intermittently inserting a catheter and removing it once the bladder is empty, which helps to reduce the risk of bladder infections. This measure is not adjusted for resident characteristics.
- Percentage of long-stay residents with new or worsened bowel or bladder incontinence.
This measure reports the percent of long-stay residents with new or worsened ability to control their bowels or bladder. Over half of nursing home residents are incontinent of urine, which can increase their risk for falls with injury and pressure ulcers/sores. Residents who are incontinent often avoid group activities due to embarrassment and may have a lower quality of life. Staff can reduce incontinence episodes by employing strategies such as bladder or bowel training and prompted or scheduled voiding. This measure is not adjusted for resident characteristics.
Health Inspections?
| Current | State Average | |
|---|---|---|
Combined Federal and State Health Inspections Rating |  (higher is better) (higher is better) |
NA |
Health Inspections
The California Department of Public Health state inspectors conduct nursing home inspections on behalf of the federal government (Centers for Medicare and Medicaid) and the state to ensure that facilities are meeting federal and state health and safety standards. Examples of standards include adequate staffing, managing medications properly, storing and preparing food properly, protecting residents from physical or mental abuse or neglect.
There are multiple types of inspections including standard health inspections that occur approximately every 9-15 months, complaint investigations, infection control investigations, and special incident investigations. CMS issues federal citations for serious health and safety violations that are found during these inspections. Similarly, the state of California issues citations to enforce the state’s nursing home quality and safety standards. Details below show the specific areas where health and safety violations occurred. Readers can use this information to ask questions of nursing home administrators about corrections the facility is making to address problem(s). Residents and family members have the right to review the inspection reports issued by CDPH.
Combined Federal and State Health Inspections Rating (Data Source: Cal Long Term Care Compare: 10/1/2022 through 9/30/2025)
This rating is based on the number and type of state and federal citations that were found during the reporting period. More weight is given to the most recent health inspection and, therefore, the most recent violations. The state may cite a facility for the same violation that the federal government identifies, while other times the federal and state violations are completely different.
Substantiated Complaints?
| Current | State Average | |
|---|---|---|
Substantiated complaints from last three years | 5 (lower is better) |
12.0 (lower is better) |
Substantiated Complaints
Complaints about nursing home quality of care may be filed with the California Department of Public Health by residents, family members, nursing home staff, or long term care ombudsman from the California Department of Aging. Complaints are investigated within 24 hours of a death or serious harm and 10 days for other potential violations. Complaint investigations must be completed within 60 days. These complaints may result in one or more federal and/or state citations and possible fines.
Substantiated complaints from last three years (Data Source: CMS Provider Data: 9/1/2022 through 8/31/2025)
This number represents the total number of complaints made about the facility that were substantiated by state inspectors following an investigation.
Federal Health Inspection Deficiencies?
| Current | State Average | |
|---|---|---|
Number of federal health inspection deficiencies | 25 (lower is better) |
33.0 (lower is better) |
Dates of two most recent health inspections | 9/12/2024, 6/11/2021 |
NA |
Type, Scope and Severity of Deficiencies |
||
Freedom from abuse, neglect, and exploitation | 0 (lower is better) |
2.0 (lower is better) |
Quality of life and care | 6 (lower is better) |
8.0 (lower is better) |
Infection control | 3 (lower is better) |
2.0 (lower is better) |
Resident assessment and care planning | 4 (lower is better) |
5.0 (lower is better) |
Nursing and physician services | 2 (lower is better) |
1.0 (lower is better) |
Resident rights | 5 (lower is better) |
5.0 (lower is better) |
Nutrition and dietary | 0 (lower is better) |
4.0 (lower is better) |
Pharmacy service | 3 (lower is better) |
4.0 (lower is better) |
Environmental | 0 (lower is better) |
2.0 (lower is better) |
Administration | 2 (lower is better) |
1.0 (lower is better) |
Number of federal health inspection deficiencies | 25 (lower is better) |
33.0 (lower is better) |
Severity | ||
Immediate jeopardy to resident health or safety | 0 (lower is better) |
0.3 (lower is better) |
Actual harm | 0 (lower is better) |
0.7 (lower is better) |
Minimal harm or the potential for actual harm | 25 (lower is better) |
31.0 (lower is better) |
No harm with the potential for minimal harm | 0 (lower is better) |
1.0 (lower is better) |
Scope | ||
Many residents (potentially) affected | 0 (lower is better) |
1.6 (lower is better) |
Some residents (potentially) affected | 3 (lower is better) |
10.0 (lower is better) |
Few residents (potentially) affected | 22 (lower is better) |
22.0 (lower is better) |
Federal Health Inspection Deficiencies
This section shows details about the federal deficiencies where citations were issued for health-related violations.
Number of federal health inspection deficiencies (Data Source: CMS Health Deficiencies: see dates in the table)
This measure shows the number of federal deficiencies issued for serious violations by the nursing home based on health and infection control inspections and complaint and special incident investigations.
Dates of two most recent health inspections (Data Source: CMS Health Deficiencies: see dates in the table)
This shows the dates of the nursing home’s last two standard health inspections by the California Department of Public Health. More recent dates are better because residents and family members can be more confident that the reported measures reflect the nursing home’s current safety and quality of care and adherence to laws and regulations.
Type, Scope and Severity of Deficiencies (Data Source: CMS Health Deficiencies: see dates in the table)
Type of health deficiencies
The standard health inspection is unannounced and usually occurs approximately once per year. It covers 10 topics: Freedom from Abuse, Neglect, and Exploitation, Quality of Life and Care, Infection Control, Resident Assessment and Care Planning, Nursing and Physician Services, Pharmacy Service, Resident Rights, Nutrition and Dietary, Environmental, and Administration. This shows the number of deficiencies issued within each category.
Severity and scope of health deficiencies
CMS instructs inspectors to assess the severity and scope of health deficiencies and select the appropriate enforcement action. The severity tells us how serious the problem is. The scope tells us how common the problem is. For example, a problem affecting many residents might still be less severe than one affecting just a few if those few experienced serious harm.
Severity reflects the level of harm from a deficiency and is categorized into four levels:
- Immediate jeopardy: The situation is very serious and poses a direct threat to a resident’s health or safety, possibly leading to serious injury, harm, impairment, or even death.
- Actual harm: The problem has already caused harm, but it is not an immediate serious risk to health or safety.
- No actual harm with potential for more than minimal harm: The issue could cause more significant harm, but it is not an immediate threat.
- No actual harm with potential for minimal harm: The problem could cause minor harm but hasn’t done so yet.
Scope reflects how many residents were affected or potentially affected by a problem. It has three categories:
- Many: The problem is widespread and affects a large number of residents throughout the nursing home.
- Some: The problem affects a few residents, showing a pattern or recurring issue.
- Few: The problem affects just one or a small number of residents and doesn’t happen often.
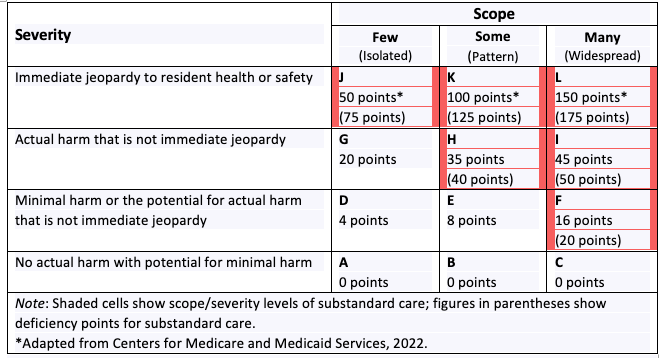
For more details about the scope and severity weights table, see: https://www.cms.gov/medicare/provider-enrollment-and-certification/certificationandcomplianc/downloads/usersguide.pdf
State Health and Safety Citations?
| Current | State Average | |
|---|---|---|
Number of class AA citations (resident death) | 0 (lower is better) |
0.1 (lower is better) |
Number of class A citations (resident danger) | 0 (lower is better) |
0.5 (lower is better) |
Number of class B citations (resident care) | 0 (lower is better) |
1.5 (lower is better) |
Total number of state citations | 0 (lower is better) |
2.0 (lower is better) |
State Health and Safety Citations
These data show the number of state citations issued for serious health and safety violations by the nursing home.
State citations are classified by severity into three categories:
- Class AA citations are the most severe and are issued when a health and safety violation by a facility has directly caused a resident’s death. Fines for Class AA citations range from $25,000 to $100,000 per incident. These citations are rare but indicate serious issues with the facility’s care.
- Class A citations are issued when residents are in imminent danger, meaning there’s a high risk of serious harm or death due to violations of state or federal laws. These citations are more serious and less common than Class B citations. Fines for Class A citations range from $2,000 to $20,000 per violation
- Class B citations are issued for health and safety violations that are less severe than Class A or AA citations. They are the most common type of citation. Fines for Class B citations range from $100 to $2,000 per violation.
Total number of state citations (Data Source: CA Health Facilities State Enforcement Actions: through 9/30/2025)
This is the total number of citations issued during the reporting period.
Federal and State Financial Penalties for Violations ?
| Current | State Average | |
|---|---|---|
Federal fines issued for violations from the last three years ($) | $0 (lower is better) |
$29,745 (lower is better) |
State fines issued for violations from the last three years ($) | NA |
$50,802 (lower is better) |
Total federal and state fines ($) | $0 (lower is better) |
$62,496 (lower is better) |
Number of days the facility was denied payment due to unresolved violations | 0 (lower is better) |
0.0 (lower is better) |
Federal and State Financial Penalties for Violations
In addition to citations, CMS or the state can also impose financial penalties on nursing homes for serious health and safety violations or for failing to fix these problems over time. Penalties can include a one-time fine, a daily fine until the issues are resolved, or restrictions like withholding Medicare payments or stopping new admissions. If a nursing home doesn’t make the necessary corrections, it might lose its federal certification or state license and be forced to close.
Federal fines issued for violations from the last three years ($) (Data Source: CMS Penalties: through 9/30/2025)
This figure shows the total dollar amount in fines that CMS has charged the nursing home for not following health and safety rules during the specified period. The amount of the fines can vary depending on how many residents were affected or the seriousness of the violation. Most nursing homes do not have any federal fines.
State fines issued for violations from the last three years ($) (Data Source: CA Health Facilities State Enforcement Actions: through 9/30/2025)
This amount represents the total dollar amount in fines charged by the California Department of Public Health (CDPH) to the nursing home for not following health and safety rules during the specified period. Most nursing homes do not receive state fines.
Total federal and state fines ($) (Data Source: CMS Penalties; CA Health Facilities State Enforcement Actions: through 9/30/2025)
This is the total dollar amount charged to the nursing home for not following federal and/or state health and safety rules. Most nursing homes do not have any federal or state fines.
Number of days the facility was denied payment due to unresolved violations (Data Source: CMS Penalties: through 9/30/2025)
This is the number of days the nursing home could not receive Medicare payments for new residents because of unresolved violations. Most nursing homes do not have any denials of payment.
Fire Safety and Emergency Preparedness Inspections?
| Current | State Average | |
|---|---|---|
Total number of fire safety and emergency preparedness citations | 21 (lower is better) |
14.0 (lower is better) |
Date of most recent fire safety and emergency preparedness inspection | 9/17/2024 |
NA |
Fire Safety and Emergency Preparedness Inspections
Total number of fire safety and emergency preparedness citations (Data Source: CMS Fire Safety Deficiencies: see date in the table)
This is the nursing home’s total number of fire safety and emergency preparedness citations reported from their last two inspections. Federal law requires annual fire safety inspections and requires nursing homes to provide the results of the most recent inspection for public review. Inspections cover 18 different topic areas: Smoke, Emergency Preparedness, Gas and Vacuum and Electrical Systems, Egress, Services Construction, Electrical, Automatic Sprinkler Systems, Corridor Walls and Doors, Emergency Plans and Fire Drills, Fire Alarm Systems, Interior, Hazardous Area, Illumination and Emergency Power, Laboratories, Medical Gases and Anaesthetizing Areas, Smoking Regulations, Miscellaneous.


